A HEAD IS A TERRIBLE THING TO WASTE
Stiff
The way I see it, being dead is not terribly far off from being on a cruise ship. Most of your time is spent lying on your back. The brain has shut down. The flesh begins to soften. Nothing much new happens, and nothing is expected of you.
If I were to take a cruise, I would prefer that it be one of those research cruises, where the passengers, while still spending much of the day lying on their backs with blank minds, also get to help out with a scientist’s research project. These cruises take their passengers to unknown, unimagined places. They give them the chance to do things they would not otherwise get to do.
I guess I feel the same way about being a corpse. Why lie around on your back when you can do something interesting and new, something useful ?
For every surgical procedure developed, from heart transplants to gender reassignment surgery, cadavers have been there alongside the surgeons, making history in their own quiet, sundered way. For two thousand years, cadavers–some willingly, some unwittingly–have been involved in science’s boldest strides and weirdest undertakings. Cadavers were around to help test France’s first guillotine, the “humane” alternative to hanging. They were there at the labs of Lenin’s embalmers, helping test the latest techniques. They’ve been there (on paper) at Congressional hearings, helping make the case for mandatory seat belts. They’ve ridden the Space Shuttle (okay, pieces of them), helped a graduate student in Tennessee debunk spontaneous human combustion, been crucified in a Parisian laboratory to test the authenticity of the Shroud of Turin.
In exchange for their experiences, these cadavers agree to a sizable amount of gore. They are dismembered, cut open, rearranged. But here’s the thing: They don’t endure anything. Cadavers are our superheros: They brave fire without flinching, withstand falls from tall buildings and head‑on car crashes into walls. You can fire a gun at them or run a speedboat over their legs, and it will not faze them. Their heads can be removed with no deleterious effect. They can be in six places at once. I take the Superman point of view: What a shame to waste these powers, to not use them for the betterment of humankind.
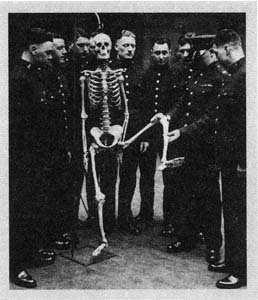
This is a book about notable achievements made while dead. There are people long forgotten for their contributions while alive, but immortalized in the pages of books and journals. On my wall is a calendar from the Mütter Museum at the College of Physicians of Philadelphia. The photograph for October is of a piece of human skin, marked up with arrows and tears; it was used by surgeons to figure out whether an incision would be less likely to tear if it ran lengthwise or crosswise. To me, ending up an exhibit in the Mütter Museum or a skeleton in a medical school classroom is like donating money for a park bench after you’re gone: a nice thing to do, a little hit of immortality. This is a book about the sometimes odd, often shocking, always compelling things cadavers have done.
Not that there’s anything wrong with just lying around on your back. In its way, rotting is interesting too, as we will see. It’s just that there are other ways to spend your time as a cadaver. Get involved with science.
Be an art exhibit. Become part of a tree. Some options for you to think about.
Death. It doesn’t have to be boring.
There are those who will disagree with me, who feel that to do anything other than bury or cremate the dead is disrespectful. That includes, I suspect, writing about them. Many people will find this book disrespectful. There is nothing amusing about being dead, they will say.
Ah, but there is. Being dead is absurd. It’s the silliest situation you’ll find yourself in. Your limbs are floppy and uncooperative. Your mouth hangs open. Being dead is unsightly and stinky and embarrassing, and there’s not a damn thing to be done about it.
This book is not about death as in dying. Death, as in dying, is sad and profound. There is nothing funny about losing someone you love, or about being the person about to be lost. This book is about the already dead, the anonymous, behind‑the‑scenes dead. The cadavers I have seen were not depressing or heart‑wrenching or repulsive. They seemed sweet and well‑intentioned, sometimes sad, occasionally amusing. Some were beautiful, some monsters. Some wore sweatpants and some were naked, some in pieces, others whole.
All were strangers to me. I would not want to watch an experiment, no matter how interesting or important, that involved the remains of someone I knew and loved. (There are a few who do. Ronn Wade, who runs the anatomical gifts program at the University of Maryland at Baltimore, told me that some years back a woman whose husband had willed his body to the university asked if she could watch the dissection. Wade gently said no.) I feel this way not because what I would be watching is disrespectful, or wrong, but because I could not, emotionally, separate that cadaver from the person it recently was. One’s own dead are more than cadavers, they are place holders for the living. They are a focus, a receptacle, for emotions that no longer have one. The dead of science are always strangers.[1]
Let me tell you about my first cadaver. I was thirty‑six, and it was eighty‑one. It was my mother’s. I notice here that I used the possessive “my mother’s,” as if to say the cadaver that belonged to my mother, not the cadaver that was my mother. My mom was never a cadaver; no person ever is. You are a person and then you cease to be a person, and a cadaver takes your place. My mother was gone. The cadaver was her hull. Or that was how it seemed to me.
It was a warm September morning. The funeral home had told me and my brother Rip to show up there about an hour before the church service.
We thought there were papers to fill out. The mortician ushered us into a large, dim, hushed room with heavy drapes and too much air‑conditioning. There was a coffin at one end, but this seemed normal enough, for a mortuary. My brother and I stood there awkwardly. The mortician cleared his throat and looked toward the coffin. I suppose we should have recognized it, as we’d picked it out and paid for it the day before, but we didn’t. Finally the man walked over and gestured at it, bowing slightly, in the manner of a maître d’ showing diners to their table. There, just beyond his open palm, was our mother’s face. I wasn’t expecting it. We hadn’t requested a viewing, and the memorial service was closed‑coffin. We got it anyway. They’d shampooed and waved her hair and made up her face. They’d done a great job, but I felt taken, as if we’d asked for the basic carwash and they’d gone ahead and detailed her.
Hey, I wanted to say, we didn’t order this. But of course I said nothing. Death makes us helplessly polite.
The mortician told us we had an hour with her, and quietly retreated. Rip looked at me. An hour ? What do you do with a dead person for an hour?
Mom had been sick for a long time; we’d done our grieving and crying and saying goodbye. It was like being served a slice of pie you didn’t want to eat. We felt it would be rude to leave, after all the trouble they’d gone to. We walked up to the coffin for a closer look. I placed my palm on her forehead, partly as a gesture of tenderness, partly to see what a dead person felt like. Her skin was cold the way metal is cold, or glass.
A week ago at that time, Mom would have been reading the Valley News and doing the Jumble. As far as I know, she’d done the Jumble every morning for the past forty‑five years. Sometimes in the hospital, I’d get up on the bed with her and we’d work on it together. She was bedridden, and it was one of the last things she could still do and enjoy. I looked at Rip. Should we all do the Jumble together one last time? Rip went out to the car to get the paper. We leaned on the coffin and read the clues aloud.
That was when I cried. It was the small things that got to me that week: finding her bingo winnings when we cleaned out her dresser drawers, emptying the fourteen individually wrapped pieces of chicken from her freezer, each one labeled “chicken” in her careful penmanship. And the Jumble. Seeing her cadaver was strange, but it wasn’t really sad. It wasn’t her .
What I found hardest to get used to this past year was not the bodies I saw, but the reactions of people who asked me to tell them about my book. People want to be excited for you when they hear you are writing a book; they want to have something nice to say. A book about dead bodies is a conversational curveball. It’s all well and good to write an article about corpses, but a full‑size book plants a red flag on your character. We knew Mary was quirky, but now we’re wondering if she’s, you know, okay . I experienced a moment last summer at the checkout desk at the medical school library at the University of California, San Francisco, that sums up what it is like to write a book about cadavers. A young man was looking at the computer record of the books under my name: The Principles and Practice of Embalming, The Chemistry of Death, Gunshot Injuries . He looked at the book I now wished to check out: Proceedings of the Ninth Stapp Car Crash Conference . He didn’t say anything, but he didn’t need to. It was all there in his glance. Often when I checked out a book I expected to be questioned. Why do you want this book? What are you up to? What kind of person are you?
They never asked, so I never told them. But I’ll tell you now. I’m a curious person. Like all journalists, I’m a voyeur. I write about what I find fascinating. I used to write about travel. I traveled to escape the known and the ordinary. The longer I did this, the farther afield I had to go. By the time I found myself in Antarctica for the third time, I began to search closer at hand. I began to look for the foreign lands between the cracks.
Science was one such land. Science involving the dead was particularly foreign and strange and, in its repellent way, enticing. The places I traveled to this past year were not as beautiful as Antarctica, but they were as strange and interesting and, I hope, as worthy of sharing.
A HEAD IS A TERRIBLE THING TO WASTE
Practicing Surgery on the Dead

The human head is of the same approximate size and weight as a roaster chicken. I have never before had occasion to make the comparison, for never before today have I seen a head in a roasting pan. But here are forty of them, one per pan, resting faceup on what looks to be a small pet‑food bowl. The heads are for plastic surgeons, two per head, to practice on. I’m observing a facial anatomy and face‑lift refresher course, sponsored by a southern university medical center and led by a half‑dozen of America’s most sought‑after face‑lifters.
The heads have been put in roasting pans–which are of the disposable aluminum variety–for the same reason chickens are put in roasting pans: to catch the drippings. Surgery, even surgery upon the dead, is a tidy, orderly affair. Forty folding utility tables have been draped in lavender plastic cloths, and a roasting pan is centered on each. Skin hooks and retractors are set out with the pleasing precision of restaurant cutlery. The whole thing has the look of a catered reception. I mention to the young woman whose job it was to set up the seminar this morning that the lavender gives the room a cheery sort of Easter‑party feeling. Her name is Theresa. She replies that lavender was chosen because it’s a soothing color.
It surprises me to hear that men and women who spend their days pruning eyelids and vacuuming fat would require anything in the way of soothing, but severed heads can be upsetting even to professionals.
Especially fresh ones (“fresh” here meaning unembalmed). The forty heads are from people who have died in the past few days and, as such, still look very much the way they looked while those people were alive. (Embalming hardens tissues, making the structures less pliable and the surgery experience less reflective of an actual operation.)
For the moment, you can’t see the faces. They’ve been draped with white cloths, pending the arrival of the surgeons. When you first enter the room, you see only the tops of the heads, which are shaved down to stubble. You could be looking at rows of old men reclining in barber chairs with hot towels on their faces. The situation only starts to become dire when you make your way down the rows. Now you see stumps, and the stumps are not covered. They are bloody and rough. I was picturing something cleanly sliced, like the edge of a deli ham. I look at the heads, and then I look at the lavender tablecloths. Horrify me, soothe me, horrify me.
They are also very short, these stumps. If it were my job to cut the heads off bodies, I would leave the neck and cap the gore somehow. These heads appear to have been lopped off just below the chin, as though the cadaver had been wearing a turtleneck and the decapitator hadn’t wished to damage the fabric. I find myself wondering whose handiwork this is.
“Theresa?” She is distributing dissection guides to the tables, humming quietly as she works.
“Mm?”
“Who cuts off the heads?”
Theresa answers that the heads are sawed off in the room across the hall, by a woman named Yvonne. I wonder out loud whether this particular aspect of Yvonne’s job bothers her. Likewise Theresa. It was Theresa who brought the heads in and set them up on their little stands. I ask her about this.
“What I do is, I think of them as wax.”
Theresa is practicing a time‑honored coping method: objectification. For those who must deal with human corpses regularly, it is easier (and, I suppose, more accurate) to think of them as objects, not people. For most physicians, objectification is mastered their first year of medical school, in the gross anatomy lab, or “gross lab,” as it is casually and somewhat aptly known. To help depersonalize the human form that students will be expected to sink knives into and eviscerate, anatomy lab personnel often swathe the cadavers in gauze and encourage students to unwrap as they go, part by part.
The problem with cadavers is that they look so much like people. It’s the reason most of us prefer a pork chop to a slice of whole suckling pig. It’s the reason we say “pork” and “beef” instead of “pig” and “cow.” Dissection and surgical instruction, like meat‑eating, require a carefully maintained set of illusions and denial. Physicians and anatomy students must learn to think of cadavers as wholly unrelated to the people they once were.
“Dissection,” writes historian Ruth Richardson in Death, Dissection, and the Destitute , “requires in its practitioners the effective suspension or suppression of many normal physical and emotional responses to the wilful mutilation of the body of another human being.”
Heads–or more to the point, faces–are especially unsettling. At the University of California, San Francisco, in whose medical school anatomy lab I would soon spend an afternoon, the head and hands are often left wrapped until their dissection comes up on the syllabus. “So it’s not so intense,” one student would later tell me. “Because that’s what you see of a person.”
The surgeons are beginning to gather in the hallway outside the lab, filling out paperwork and chatting volubly. I go out to watch them. Or to not watch the heads, I’m not sure which. No one pays much attention to me, except for a small, dark‑haired woman, who stands off to the side, staring at me. She doesn’t look as if she wants to be my friend. I decide to think of her as wax. I talk with the surgeons, most of whom seem to think I’m part of the setup staff. A man with a shrubbery of white chest hair in the V‑neck of his surgical scrubs says to me: “Were y’in there injectin’ ’em with water?” A Texas accent makes tarry of his syllables. “Plumpin’ ’em up?” Many of today’s heads have been around a few days and have, like any refrigerated meat, begun to dry out. Injections of saline, he explains, are used to freshen them.
Abruptly, the hard‑eyed wax woman is at my side, demanding to know who I am. I explain that the surgeon in charge of the symposium invited me to observe. This is not an entirely truthful rendering of the events. A entirely truthful rendering of the events would employ words such as “wheedle.,” “plead,” and “attempted bribe.”
“Does publications know you’re here? If you’re not cleared through the publications office, you’ll have to leave.” She strides into her office and dials the phone, staring at me while she talks, like security guards in bad action movies just before Steven Seagal clubs them on the head from behind.
One of the seminar organizers joins me. “Is Yvonne giving you a hard time?”
Yvonne! My nemesis is none other than the cadaver beheader. As it turns out, she is also the lab manager, the person responsible when things go wrong, such as writers fainting and/or getting sick to their stomach and then going home and writing books that refer to anatomy lab managers as beheaders. Yvonne is off the phone now. She has come over to outline her misgivings. The seminar organizer reassures her. My end of the conversation takes place entirely in my head and consists of a single repeated line. You cut off heads. You cut off heads. You cut off heads .
Meanwhile, I’ve missed the unveiling of the faces. The surgeons are already at work, leaning kiss‑close over their specimens and glancing up at video monitors mounted above each work station. On the screen are the hands of an unseen narrator, demonstrating the procedures on a head of his own. The shot is an extreme close‑up, making it impossible to tell, without already knowing, what kind of flesh it is. It could be Julia Child skinning poultry before a studio audience.
The seminar begins with a review of facial anatomy. “Elevate the skin in a subcutaneous plane from lateral to medial,” intones the narrator.
Obligingly, the surgeons sink scalpels into faces. The flesh gives no resistance and yields no blood.
“Isolate the brow as a skin island.” The narrator speaks slowly, in a flat tone. I’m sure the idea is to sound neither excited and delighted at the prospect of isolating skin islands, nor overly dismayed. The net effect is that he sounds chemically sedated, which seems to me like a good idea.
I walk up and down the rows. The heads look like rubber Halloween masks. They also look like human heads, but my brain has no precedent for human heads on tables or in roasting pans or anywhere other than on top of human bodies, and so I think it has chosen to interpret the sight in a more comforting manner. Here we are at the rubber mask factory. Look at the nice men and women working on the masks . I used to have a Halloween mask of an old toothless man whose lips fell in upon his gums. There are several of him here. There is a Hunchback of Notre Dame, bat‑nosed and with lower teeth exposed, and a Ross Perot.
The surgeons don’t seem queasy or repulsed, though Theresa told me later that one of them had to leave the room. “They hate it,” she says. “It” meaning working with heads. I sense from them only a mild discomfort with their task. As I stop at their tables to watch, they turn to me with a vaguely irritated, embarrassed look. You’ve seen that look if you make a habit of entering bathrooms without knocking. The look says, Please go away.
Though the surgeons clearly do not relish dissecting dead people’s heads, they just as clearly value the opportunity to practice and explore on someone who isn’t going to wake up and look in the mirror anytime soon. “You have a structure you keep seeing [during surgeries], and you’re not sure what it is, and you’re afraid to cut it,” says one surgeon. “I came here with four questions.” If he leaves today with answers, it will have been worth the $500. The surgeon picks his head up and sets it back down, adjusting its position like a seamstress pausing to shift the cloth she is working on. He points out that the heads aren’t cut off out of ghoulishness. They are cut off so that someone else can make use of the other pieces: arms, legs, organs. In the world of donated cadavers, nothing is wasted. Before their face‑lifts, today’s heads got nose jobs in the Monday rhinoplasty lab.
It’s the nose jobs that I trip over. Kindly, dying southerners willed their bodies for the betterment of science, only to end up as practice runs for nose jobs? Does it make it okay that the kindly southerners, being dead kindly southerners, have no way of knowing that this is going on? Or does the deceit compound the crime? I spoke about this later with Art Dalley, the director of the Medical Anatomy Program at Vanderbilt University in Nashville and an expert in the history of anatomical gift‑giving. “I think there’s a surprising number of donors who really don’t care what happens to them,” Dalley told me. “To them it’s just a practical means of disposing of a body, a practical means that fortunately has a ring of altruism.”
Though it’s harder to justify the use of a cadaver for practicing nose jobs than it is for practicing coronary bypasses, it is justifiable nonetheless.
Cosmetic surgery exists, for better or for worse, and it’s important, for the sake of those who undergo it, that the surgeons who do it are able to do it well. Though perhaps there ought to be a box for people to check, or not check, on their body donor form: Okay to use me for cosmetic purposes. [2]
I sit down at Station 13, with a Canadian surgeon named Marilena Marignani. Marilena is dark‑haired, with large eyes and strong cheekbones. Her head (the one on the table) is gaunt, with a similarly strong set to the bones. It’s an odd way for the two women’s lives to intersect; the head doesn’t need a face‑lift, and Marilena doesn’t usually do them. Her practice is primarily reconstructive plastic surgery. She has done only two face‑lifts before and wants to hone her skills before undertaking a procedure on a friend. She wears a mask over her nose and mouth, which is surprising, because a severed head is in no danger of infection. I ask whether this is more for her own protection, a sort of psychological barrier.
Marilena replies that she doesn’t have a problem with heads. “For me, hands are hard.” She looks up from what she’s doing. “Because you’re holding this disconnected hand, and it’s holding you back.” Cadavers occasionally effect a sort of accidental humanness that catches the medical professional off guard. I once spoke to an anatomy student who described a moment in the lab when she realized the cadaver’s arm was around her waist. It becomes difficult, under circumstances such as these, to retain one’s clinical remove.
I watch Marilena gingerly probing the woman’s exposed tissue. What she is doing, basically, is getting her bearings: learning–in a detailed, hands‑on manner–what’s what and what’s where in the complicated layering of skin, fat, muscle, and fascia that makes up the human cheek. While early face‑lifts merely pulled the skin up and stitched it, tightened, into place, the modern face‑lift lifts four individual anatomical layers. This means all of these layers must be identified, surgically separated from their neighbors, individually repositioned, and sewn into place–all the while taking care not to sever vital facial nerves. With more and more cosmetic procedures being done endoscopically–by introducing tiny instruments through a series of minimally invasive incisions–knowing one’s way around the anatomy is even more critical. “With the older techniques, they peeled everything down and they could see it all in front of them,” says Ronn Wade, director of the Anatomical Services Division of the University of Maryland School of Medicine. “Now when you go in with a camera and you’re right on top of something, it’s harder to keep yourself oriented.”
Marilena’s instruments are poking around the edges of a glistening yolk‑colored blob. The blob is known among plastic surgeons as the malar fat pad. “Malar” means relating to the cheek. The malar fat pad is the cushion of youthful padding that sits high on your cheekbone, the thing grandmothers pinch. Over the years, gravity coaxes the fat from its roost, and it commences a downward slide, piling up at the first anatomical roadblock it reaches: the nasolabial folds (the anatomical parentheses that run from the edges of a middle‑aged nose down to the corners of the mouth). The result is that the cheeks start to look bony and sunken, and bulgy parentheses of fat reinforce the nasolabial lines. During face‑lifts, surgeons put the malar fat pad back up where it started out.
“This is great,” says Marilena. “Beautiful. Just like real, but no bleeding. You can really see what you’re doing.”
Though surgeons in all disciplines benefit from the chance to try out new techniques and new equipment on cadaveric specimens, fresh parts for surgical practice are hard to come by. When I telephoned Ronn Wade in his office in Baltimore, he explained that the way most willed body programs are set up, anatomy labs have first priority when a cadaver comes in. And even when there’s a surplus, there may be no infrastructure in place to get the bodies from the anatomy department of the medical school over to the hospitals where the surgeons are– and no place at the hospital for a surgical practice lab. At Marilena’s hospital, surgeons typically get body parts only when there’s been an amputation.
Given the frequency of human head amputations, an opportunity like today’s would be virtually nonexistent outside of a seminar.
Wade has been working to change the system. He is of the opinion–and it’s hard to disagree with him–that live surgery is the worst place for a surgeon to be practicing a new skill. So he got together with the heads–sorry, chiefs –of surgery at Baltimore’s hospitals and worked out a system. “When a group of surgeons want to get together and try out, say, some new endoscopic technique, they call me and I set it up.” Wade charges a nominal fee for the use of the lab, plus a small per‑cadaver fee.
Two‑thirds of the bodies Wade takes in now are being used for surgical practice.
I was surprised to learn that even when surgeons are in residencies, they aren’t typically given an opportunity to practice operations on donated cadavers. Students learn surgery the way they have always learned: by watching experienced surgeons at work. At teaching hospitals affiliated with medical schools, patients who undergo surgery typically have an audience of interns. After watching an operation a few times, the intern is invited to step in and try his or her hand, first on simple maneuvers such as closures and retractions, and gradually at more complicated steps. “It’s basically on‑the‑job training,” says Wade. “It’s an apprenticeship.”
It has been this way since the early days of surgery, the teaching of the craft taking place largely in the operating room. Only in the past century, however, has the patient routinely stood to gain from the experience.
Nineteenth‑century operating “theaters” had more to do with medical instruction than with saving patients’ lives. If you could, you stayed out of them at all cost.
For one thing, you were being operated on without anesthesia. (The first operations under ether didn’t take place until 1846.) Surgical patients in the late 1700s and early 1800s could feel every cut, stitch, and probing finger. They were often blindfolded–this may have been optional, not unlike the firing squad hood–and invariably bound to the operating table to keep them from writhing and flinching or, quite possibly, leaping from the table and fleeing into the street. (Perhaps owing to the presence of an audience, patients underwent surgery with most of their clothes on.)
The early surgeons weren’t the hypereducated cowboy‑saviors they are today. Surgery was a new field, with much to be learned and near‑constant blunders. For centuries, surgeons had shared rank with barbers, doing little beyond amputations and tooth pullings, while physicians, with their potions and concoctions, treated everything else. (Interestingly, it was proctology that helped pave the way for surgery’s acceptance as a respectable branch of medicine. In 1687, the king of France was surgically relieved of a painful and persistent anal fistula and was apparently quite grateful for, and vocal about, his relief.)
Nepotism, rather than skill, secured a post at early‑nineteenth‑century teaching hospitals. The December 20, 1828, issue of The Lancet contains excerpts from one of the earliest surgical malpractice trials, which centered on the incompetency of one Bransby Cooper, nephew of the famed anatomist Sir Astley Cooper. Before an audience of some two hundred colleagues, students, and onlookers, the young Cooper proved beyond question that his presence in the operating theater owed everything to his uncle and nothing to his talents. The operation was a simple bladder stone removal (lithotomy) at London’s Guy’s Hospital; the patient, Stephen Pollard, was a hardy working‑class man. While lithotomies were normally completed in a matter of minutes, Pollard was on the table for an hour, with his knees at his neck and his hands bound to his feet while the clueless medic tried in vain to locate the stone. “A blunt gorget was also introduced, and the scoop, and several pair of forceps,” recalled one witness. Another described the “horrible squash, squash of the forceps in the perineum.” When a succession of tools failed to produce the stone, Cooper “introduced his finger with some force…” It was around this point that Pollard’s endurance[3]ran dry. “Oh! Let it go!”
he is quoted as saying. “Pray let it keep in!” Cooper persisted, cursing the man’s deep perineum (in fact, an autopsy showed it to be a quite normally proportioned perineum). After digging with his finger for some ungodly amount of time, he got up from his seat and “measured fingers with those of other gentlemen, to see if any of them had a longer finger.”
Eventually he went back to his toolkit and, with forceps, conquered the recalcitrant rock–a relatively small one, “not larger than a common Windsor bean”–brandishing it above his head like an Academy Award winner. The quivering, exhausted mass that was Stephen Pollard was wheeled to a bed, where he died of infection and God knows what else twenty‑nine hours later.
Bad enough that some ham‑handed fop in a waistcoat and bowtie was up to his wrists in your urinary tract, but on top of that you had an audience–not just the young punters from the medical school but, judging from a description of another lithotomy at Guy’s Hospital in an 1829 Lancet , half the city: “Surgeons and surgeons’ friends… French visitors, and interlopers filled the space around the table… There was soon a general outcry throughout the gallery and upper rows–‘hat’s off,’ ‘down heads,’ …was loudly vociferated from different parts of the theatre.”
The cabaret atmosphere of early medical instruction began centuries before, in the standing‑room‑only dissecting halls of the renowned Italian medical academies of Padua and Bologna. According to C. D. O’Malley’s biography of the great Renaissance anatomist Andreas Vesalius, one enthusiastic spectator at a crowded Vesalius dissection, bent on a better view, leaned too far out and tumbled from his bench to the dissecting platform below. “Because of his accidental fall… the unfortunate Master Carlo is unable to attend and is not very well,” read the note proffered at the next lecture. Master Carlo, one can be sure, did not seek treatment at the place he went for lectures.
Without exception, the only people who checked themselves in at teaching hospitals were those too poor to pay for private surgery. In return for an operation that was as likely to kill them as make them better–bladder stone removal had a mortality rate of 50 percent–the poor basically donated themselves as living practice material. Not only were the surgeons unskilled, but many of the operations being done were purely experimental–no one really expected them to help. Wrote historian Ruth Richardson in Death, Dissection, and the Destitute , “The benefit [to the patient] was often incidental to the experiment.”
With the advent of anesthesia, patients were at least unconscious while the young resident tried his hand at a new procedure. But they probably didn’t give their permission for a trainee to take the helm. In the heady days before consent forms and drop‑of‑a‑hat lawsuits, patients didn’t realize what they might be in for if they underwent surgery at a teaching hospital, and doctors took advantage of this fact. While a patient was under, a surgeon might invite a student to practice an appendectomy.
Never mind that the patient didn’t have appendicitis. One of the more common transgressions was the gratuitous pelvic exam. A budding M.D.’s first Pap smear–the subject of significant anxiety and dread‑–was often administered to an unconscious female surgical patient. (Nowadays, enlightened medical schools will hire a “pelvic educator,” a sort of professional vagina who allows the students to practice on her and offers personalized feedback and is, in my book anyway, a nominee for sainthood.)
Gratuitous medical procedures happen far less than they used to, owing to the public’s growing awareness. “Patients are savvier these days, and the climate has changed a great deal,” Hugh Patterson, who runs the willed body program at the University of California, San Francisco, Medical School, told me. “Even at a teaching hospital, patients request that residents not do the surgery. They want to be assured the attending does the procedure. It makes training very difficult.”
Patterson would like to see specialized cadaver anatomy labs added to third‑ and fourth‑year programs–instead of teaching anatomy only in the first year, “as one big bolus.” Already, he and his colleagues have added a focused dissection, similar to the facial anatomy lab I’m observing today, to the curricula of surgical subspecialties. They’ve also set up a series of sessions at the medical school morgue to teach emergency room procedures to third‑year students. Before a cadaver is embalmed and delivered to the anatomy lab, it may pass an afternoon getting tracheal intubations and catheterizations. (Some schools use anesthetized dogs for this purpose.) Given the urgency and difficulty of certain ER procedures, it makes good sense to practice them first on the dead. In the past, this has been done in a less formal manner, on freshly dead hospital patients, without consent–a practice whose propriety is intermittently debated in hushed meetings of the American Medical Association. They should probably just ask for permission: According to one New England Journal of Medicine study on the subject, 73 percent of parents of newly dead children, when asked, gave consent to use their child’s body for teaching intubation skills.
I ask Marilena if she plans to donate her remains. I have always assumed that a sense of reciprocity prompts doctors to donate– repayment for the generosity of the people they dissected in medical school. Marilena, for one, isn’t going to. She cites a lack of respect. It surprises me to hear her say this. As far as I can tell, the heads are being treated with respect. I hear no joking or laughter or callous comments. If there can be a respectful way to “deglove” a face, if loosening the skin of someone’s forehead and flipping it back over his or her eyes can be a respectful act, then I think these people are managing it. It’s strictly business.
It turns out that what Marilena objected to was a couple of the surgeons’ taking photographs of their cadaver heads. When you take a photograph of a patient for a medical journal, she points out, you have the patient sign a release. The dead can’t refuse to sign releases, but that doesn’t mean they wouldn’t want to. This is why cadavers in photographs in pathology and forensics journals have black bars over their eyes, like women on the Dos and Don’ts pages of Glamour . You have to assume that people don’t want to be photographed dead and dismembered, any more than they want to be photographed naked in the shower or asleep on a plane with their mouth hanging open.
Most doctors aren’t worried about a lack of respect from other doctors.
Most of the ones I’ve spoken to would worry, if anything, about a lack of respect from students in the first‑year gross anatomy lab–my next stop.
The seminar is nearly over. The video monitors are blank and the surgeons are cleaning up and filing out into the hallway. Marilena replaces the white cloth on her cadaver’s face; about half the surgeons do this. She is conscientiously respectful. When I asked her why the eyes of the dead woman had no pupils, she did not answer, but reached up and closed the eyelids. As she slides back her chair, she looks down at the benapkined form and says, “May she rest in peace.” I hear it as “pieces,” but that’s just me.
Äàòà äîáàâëåíèÿ: 2015-05-08; ïðîñìîòðîâ: 2331;
