Umbilical and Paraumbilical hernia
An umbilical hernia is the result of improper healing of an umbilical scar, which leads to a fascial defect that is covered by skin. If the defect is to one side, it is called a paraumbilical hernia; this variant is more common in adults. The vast majority of umbilical hernias presenting in children are congenital, whereas 90% of those diagnosed in adults are acquired. These hernias are eight times more common in black children than in white ones.
The onset of umbilical or paraumbilical hernia in older patients is usually sudden, and the defect tends to be relatively small. In these patients, it is important to look for an underlying cause of increased intra-abdominal pressure (e.g., ascites or an intra-abdominal tumor).
The differential diagnosis of an umbilical hernia should include so-called caput medusae, a condition in which varicosities extend radially from the umbilicus as a consequence of portal hypertension.
Another condition to be considered is the so-called Sister Mary Joseph node, which is a metastatic deposit of intra-abdominal cancer at the umbilicus. The cancer cells reach this region via lymphatic vessels in the falciform ligament.
Other periumbilical masses that might be confused with an umbilical hernia are umbilical granulomas, omphalomesenteric duct remnant cysts, and urachal cysts.
Most of the defects are small and can therefore be closed by simple suturing. Alternatively, the Mayo technique may be used (fig. 28).
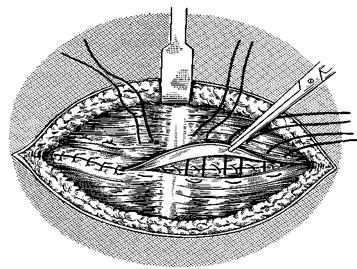
Figure 28 – Mayo technique
A subumbilical semilunar incision is made, the hernial sac is opened, the contents of the sac are reduced into the abdomen, and the sac is excised. An overlapping or waist-coating technique is then employed, in which the upper edge of the linea alba is placed so as to overlap the lower and fixed in place with a nonabsorbable mattress suture. This technique is controversial: some surgeons argue that the overlapping layers serve only to increase the tension on the repair, thus inviting recurrence.
The fascial defect is then bridged with prosthesis without fear of contact with the intra-abdominal viscera. The prosthesis is sutured circumferentially to the defect; alternatively, it can be sutured to the undersurface of the posterior rectus sheath and the linea alba above the peritoneal closure. If the peritoneum cannot be kept intact beneath the defect, omentum should be tacked to the peritoneum circumferentially to isolate the abdominal viscera from the prosthesis at least to some degree.
Дата добавления: 2015-07-04; просмотров: 1877;
